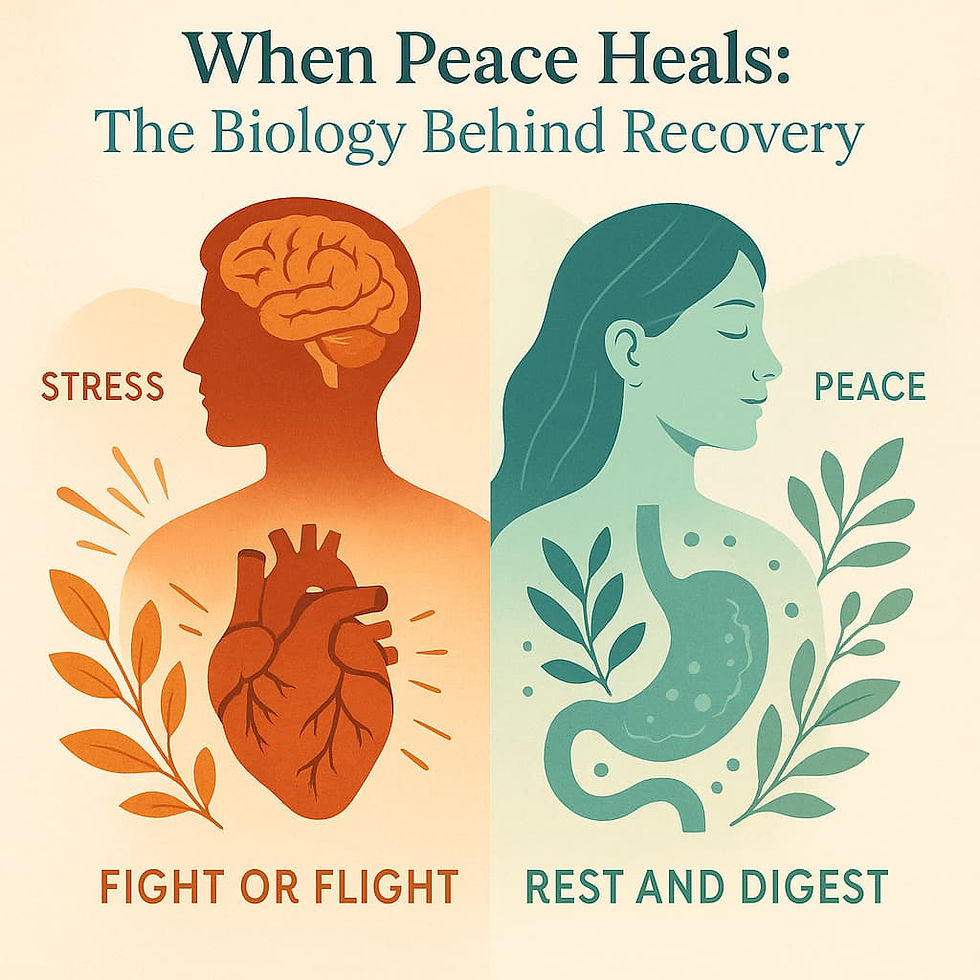
When Peace Heals: The Biology Behind Recovery
- Clark R. Mollenhoff III M.Ac., L.Ac.

- Jul 23, 2025
- 5 min read
In a previous article, we explored a subtle but powerful truth: that much of the suffering around pain isn’t just physical. It’s emotional, psychological, or existential. The panic, helplessness, and confusion about what pain means can create a second layer of suffering that’s often harder to resolve than the original issue.
This article dives a bit deeper into the body itself, and the internal mechanisms at play. The way we relate to pain isn’t just philosophical or psychological. It has profound biological consequences.
When we shift from stress and fear into calm and safety, we aren’t just “feeling better.” We are activating a radically different set of systems in the body. Systems that prioritize healing, regeneration, and internal repair.
Understanding these systems may change the way you view not only pain, but the very nature of healing itself.
The Stress Response: A Master Switch for Survival
When the body detects a threat—real or perceived—it activates the sympathetic nervous system (SNS), launching what is commonly known as the “fight, flight, or freeze” response. This reaction initiates a well-coordinated cascade through the hypothalamic-pituitary-adrenal (HPA) axis, one of the body’s primary systems for managing acute stress.
Here’s how it works: the hypothalamus releases corticotropin-releasing hormone (CRH), which signals the pituitary gland to produce adrenocorticotropic hormone (ACTH). This, in turn, stimulates the adrenal glands to release a surge of stress hormones, including cortisol (a glucocorticoid) and adrenaline (epinephrine).
These hormones prepare the body for immediate survival. Blood glucose rises to supply quick energy. The heart rate increases, and blood pressure elevates to enhance circulation to large muscle groups. Blood is diverted away from digestion and reproduction to maximize energy for action. Repair functions are put on hold. Meanwhile, immune activity is altered—often toward short-term, pro-inflammatory responses designed to ward off immediate threats, but not to support long-term balance.
In this survival state, the body is not concerned with healing—it is focused on escaping danger. While this system is highly adaptive in short bursts, chronic activation leads to dysregulation. Over time, sustained stress can disrupt hormonal rhythms, weaken immune resilience, and suppress the very repair functions that support health and recovery.
Pain Amplification Under Stress
Pain is processed not just in the body, but in the brain—specifically within a network called the pain matrix. This includes the somatosensory cortex, insula, anterior cingulate cortex (ACC), and prefrontal cortex, among others. But in times of emotional distress, the brain's pain-processing circuits become entangled with the limbic system, particularly the amygdala.
When the amygdala is hyperactive due to fear or anxiety, pain signals are amplified.
This means stress can actually sensitize the nervous system, making pain feel more intense, more diffuse, and more persistent. This phenomenon is known as central sensitization and is implicated in conditions like fibromyalgia, irritable bowel syndrome, chronic migraines, and many forms of long-term musculoskeletal pain.
The Parasympathetic System: Healing’s Operating System
Healing, by contrast, depends on the parasympathetic nervous system (PNS)—especially the vagus nerve, which is the tenth cranial nerve and one of the longest in the body.
When activated, the vagus nerve initiates a cascade of restorative processes:
Slows heart rate and respiration
Reduces systemic inflammation (via the cholinergic anti-inflammatory pathway)
Stimulates digestion and nutrient assimilation
Supports neurogenesis and emotional regulation
Promotes tissue repair and immune surveillance
This "rest, digest, and repair" mode is the body’s biological healing state. Without it, even the best interventions—surgery, medication, manual therapy—can fall short, because the body lacks the internal conditions needed to integrate and regenerate.
Importantly, vagal tone (the strength and flexibility of the vagus nerve’s signaling) is now understood as a biomarker of resilience. High vagal tone is associated with better stress recovery, lower inflammation, reduced pain sensitivity, and improved mental health.
Acupuncture and the Neurobiology of Regulation
Acupuncture offers a unique and measurable way to access this healing mode. While often misunderstood as simply a pain treatment, acupuncture is increasingly being recognized as a neuro-regulatory therapy.
Mechanisms of Action:
Modulation of Brain Activity- Functional MRI studies show that acupuncture can downregulate activity in the limbic system, especially the amygdala, insula, and ACC—regions involved in both pain and emotional processing. This helps explain acupuncture’s effect on both physical discomfort and psychological distress.
Endogenous Opioid Release- Acupuncture stimulates the release of endorphins, enkephalins, and dynorphins—the body’s natural opioids—resulting in pain modulation at both spinal and supraspinal levels.
Anti-Inflammatory Signaling- Needling stimulates the hypothalamus, which can reduce pro-inflammatory cytokine production (e.g., IL-1β, TNF-α) and increase anti-inflammatory mediators such as IL-10. It also activates the vagal anti-inflammatory reflex, especially when distal points are used.
Autonomic Nervous System Rebalancing- Heart rate variability (HRV)—a key marker of parasympathetic activity—has been shown to improve with acupuncture, indicating a shift from sympathetic dominance to parasympathetic regulation.
Neuroplastic Effects- Chronic pain changes the brain. Acupuncture may reverse maladaptive neuroplasticity by enhancing cortical connectivity, especially in default mode and salience networks—areas involved in pain prediction and attention.
Why “Doing More” Isn’t Always the Answer
Many patients with chronic pain are caught in a cycle of over-efforting. More supplements. More therapies. More research. More willpower.
But the truth is: healing does not respond well to force. It responds to conditions—and especially to the internal state in which healing is attempted.
This is why therapies that may seem “gentle” or “passive”—such as acupuncture, meditation, breathwork, or craniosacral therapy—often trigger dramatic improvements. Not because they aggressively fix the tissue, but because they deactivate threat physiology, opening the door to the body’s own restorative intelligence.
The Clinical Implications
For clinicians and patients alike, the implications are clear:
Chronic sympathetic dominance can perpetuate or worsen pain.
Addressing nervous system state is not optional—it’s essential.
Regenerative therapies must be paired with a shift into parasympathetic physiology.
Healing requires time, but more importantly, it requires the right kind of time—time spent in a state of biological readiness.
Conclusion: Peace as Biological Prerequisite
Peace is not a mindset. It is a physiological setting—one that permits the unfolding of complex, intelligent processes the body is already designed to carry out.
If your system is locked in a chronic stress loop, no treatment will reach its full potential. When the body is reminded that it is safe, and it reclaims the parasympathetic rhythm of rest, digest, and repair, then the true work of healing can begin. Peace isn’t the absence of pain. It’s the fertile ground in which recovery becomes possible. Sometimes the hardest thing to do is to become peaceful in the presence of deep pain, and yet we must, if we are to make meaningful progress. We are then faced with a paradox of sorts. We must accept our current state fully while also finding the strength to move ourselves forward. Giving up the fight will only weaken us, and fighting without surrender will take us over the edge. First, we must find peace, then we must find strength.



Comments