When the Body Speaks: Ten Reflections from the Treatment Room
- Clark R. Mollenhoff III M.Ac., L.Ac.

- Jul 5, 2025
- 7 min read
Updated: Jul 17, 2025

In clinical practice, certain truths echo across cases, regardless of diagnosis or technique. One of the most profound is this: physical pain often tells a deeper story.
The patterns we feel under our hands—the guarded shoulders, the breath that won’t descend, the muscles that resist release—are not always mechanical. Often, they’re expressions of something the body holds until the right conditions make it safe to let go.
Here are ten insights shaped by years in the treatment room. These are not rules or prescriptions, but quiet truths gathered from the shared space where healing unfolds—often in ways we don’t expect.
1. Pain as a Messenger
Not all pain signals damage. It may linger without injury, appear at rest, or flare when life turns emotional. In these cases, pain may serve as a communicator—pointing to unresolved tension or emotional holding. It can surface in conversation, then ease when something is seen or named. Rather than rushing to eliminate it, there may be value in listening to what it’s trying to say.
Chronic pain, in particular, often resists simple explanations. A person may have immaculate posture, strong musculature, and no history of acute trauma, yet experience persistent discomfort. These situations challenge the biomechanical model and invite a more layered understanding. Pain can become a signal loop, amplifying itself when its underlying message is ignored or misunderstood.
Listening to pain requires a shift in orientation. Instead of seeing it as an obstacle, we can treat it as a teacher—an indicator of where attention is needed. This doesn’t mean we glorify suffering, but we do respect the intelligence of the body and its attempts to communicate. When pain is met with curiosity instead of fear or frustration, new information often surfaces.
2. The Body Holds What the Mind Avoids
Even when someone feels emotionally ready to move on, their body may still cling. Protective tension shows up in surprising places—tight jaws, clenched pelvises, breath stuck high in the chest. These patterns often reflect old instincts of self-protection, quietly persisting beneath conscious awareness.
Many people arrive in treatment saying, "I thought I was over this," or "I don't know why I'm still reacting this way." The dissonance between cognitive readiness and somatic reality is often the result of the body storing unresolved stress. Survival strategies learned early in life don’t dissolve just because we now understand them. They need to be unwound at the level where they live—in the tissues, the breath, the reflexes.
This is why treatments that integrate touch, breath, or movement can be so potent. They allow for a kind of communication that bypasses language and taps directly into the body's memory. Sometimes, the body must be shown that it is safe before it can relinquish what it’s holding. This work can be subtle, requiring patience and attunement, but the shifts can be profound.
3. The Emotional-Physical Feedback Loop
Touching a tender area or guiding a breath can sometimes stir unexpected reactions—sadness, frustration, even tremors. These moments reveal how closely emotional and physical systems are intertwined. Paying attention to these responses helps pace the session and offers clues to what lies underneath.
This loop is not one-directional. Just as emotions can manifest physically, physical interventions can evoke emotion. A light hand on the sternum can bring tears. Stretching the diaphragm might release a flood of memories. These are not random occurrences—they are evidence of the body and psyche working in concert.
Understanding this feedback loop helps practitioners avoid missteps. If a release brings tears, the goal is not to soothe it away too quickly but to remain present with what is emerging. These moments can become transformative when they are held with care, free from interpretation or agenda. They are signs that healing is occurring not just on the surface, but at the root.
4. The Limits of Cognitive Insight
Insight doesn’t always equal relief. A person might articulate their trauma with clarity yet remain physically braced. The body needs more than understanding—it needs felt experiences of safety, permission, and release. Knowledge supports healing, but rarely completes it.
There is a common belief that "if I can just understand why I feel this way, I can make it stop." While cognitive clarity can indeed bring relief, it often doesn’t reach the parts of us that are most wounded. The nervous system doesn’t respond to logic; it responds to experience. Until the body feels safe, it may continue to react as if the original threat is present.
Somatic therapies help bridge this gap. By engaging the body directly, they offer the possibility of change without the need for explanation. A person may not need to rehash every detail of their story; they may only need to experience what it feels like to breathe freely, to be touched without flinching, or to move without fear. These experiences can create new pathways of response, even in the absence of complete understanding.
5. Respecting Readiness
Uncovering the roots of tension can feel urgent—but the body unfolds on its own schedule. Sometimes, nothing seems to happen in a session because the system isn't ready. Forcing the issue can backfire. Holding respectful space, free of pressure, is often what allows readiness to emerge later.
Healing is not a linear process, and it cannot be forced into a timeline. Practitioners may feel pressure to "make something happen" in a session, but deep change often requires stillness. It requires creating conditions where the nervous system feels it has time, space, and choice.
Honoring readiness means trusting the body's pace. It also means being attuned to subtle cues—a flicker of tension, a slight shift in breath, or a moment of eye contact. These are often the precursors to release. When the practitioner stays present without pushing, the body often responds in kind, gradually revealing what it is ready to let go of.
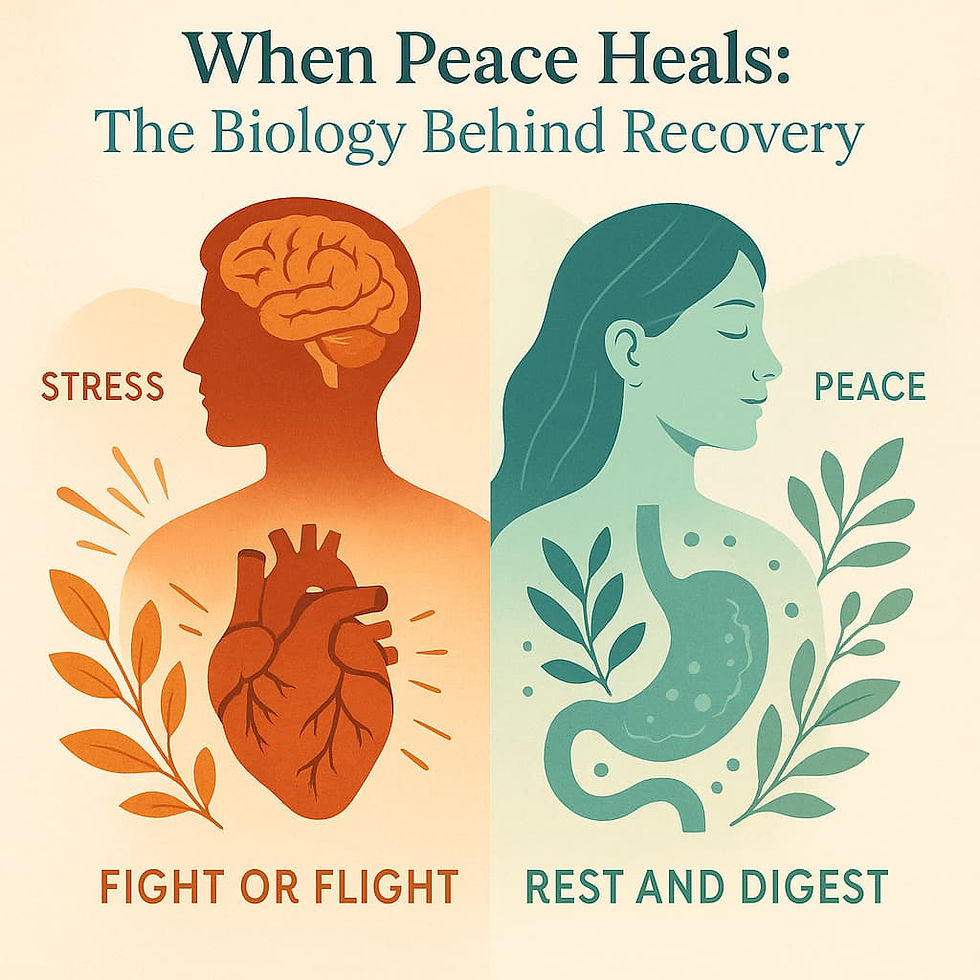
6. The Role of Somatic Safety
Softening doesn’t happen because someone is told to relax. It emerges when the body perceives safety. That perception is created through consistency, gentleness, and a total absence of threat. The tone of voice, the pace of touch, and the practitioner's internal state all contribute to this field of safety.
In a world that moves quickly, it is rare for someone to experience a space where there is no pressure to be different, to perform, or to explain. When a practitioner meets a person exactly where they are—without agenda—the body often responds with subtle signs of regulation: a longer exhale, a slight smile, a shift in gaze. These are not incidental. They are markers of the parasympathetic system coming online.
Establishing somatic safety is especially crucial when working with trauma. The body needs to know, not just intellectually but viscerally, that it is not in danger. Only then can it begin to down-regulate and access the healing states necessary for repair, integration, and transformation.
7. Micro-Releases as Markers of Progress
Healing is rarely dramatic. More often, it reveals itself in the subtlest of ways: a single tear, a quiet sigh, the release of a clenched hand. These micro-releases may seem small, but they are deeply significant. They indicate that the body is letting go—sometimes for the first time in years.
Because they can be easy to overlook, it is vital to track and validate these moments. Naming them gently can help the person build a sense of trust in the process. Over time, these small changes accumulate. The shoulders rest lower. The breath moves more freely. The person may begin to inhabit their body in a new way.
Micro-releases remind us that the nervous system changes gradually. They help practitioners and clients alike to stay engaged without chasing dramatic results. Instead, we learn to honor each opening, however small, as a milestone on the path of healing.
8. Letting Go of the Need to Fix
The desire to help can sometimes become a compulsion to fix. Practitioners may feel responsible for relieving suffering, and clients may come with the hope of being "fixed." But true healing often begins when we release the urgency to solve and instead offer presence.
Sitting with discomfort—without trying to change it—can be one of the most powerful therapeutic gestures. It communicates, on a deep level, that the person is not broken and does not need to be rescued. That they are safe to be exactly as they are.
This doesn’t mean we abandon tools or techniques. But it does mean we prioritize relationship over intervention, listening over instructing. When we hold space without agenda, we invite the body to reveal its own timing and wisdom. Often, that is when the most profound shifts occur.
9. Reframing Success in Treatment
In a results-driven culture, success is often measured by the elimination of symptoms. But in the treatment room, healing can look very different. It might mean someone learns to coexist with discomfort rather than be ruled by it. Or that they begin to feel agency in a place that once felt powerless.
Symptoms are only part of the story. A person might still feel pain but report that it no longer scares them. Or that they can breathe through it, rather than fight it. These shifts in perception and relationship are deeply therapeutic—they change not just the body, but the experience of being alive in it.
Reframing success helps both practitioner and client to stay grounded. It supports a long-term view of healing as a process of reconnection, rather than a quick fix. It also makes space for the emotional, spiritual, and relational dimensions of recovery—the parts that truly make life worth living.
10. Discomfort as a Doorway
Discomfort is not always something to avoid. Sometimes, it is the doorway to the very thing that needs to be seen, felt, or acknowledged. When approached with care, areas of tension or pain can become portals to deeper awareness.
Placing gentle attention on a sore shoulder might bring up a flood of emotion. Pressure on the diaphragm might evoke a buried memory. These moments are not always explainable, but they are meaningful. The body holds memory, and under the right conditions, it may choose to release it.
Using discomfort as a doorway requires great skill and attunement. It is never about pushing through pain. Instead, it is about meeting it with respect and curiosity—being willing to listen to what it might say. In doing so, we honor the body as a wise and willing partner in healing.
These moments often arrive quietly. A subtle change mid-session, or a patient who reports a new spaciousness in an old tension. A calm that wasn’t possible before. These are significant shifts. They mean something once braced is beginning to move.
The body speaks in breath, in posture, in tension, in tremor—often before words arrive. Learning to listen opens doors to healing that move far beyond the physical.
As practitioners, we don’t always need to interpret or fix. Sometimes it’s enough to notice. To stay present. And to trust in the quiet intelligence of the body at work.


Comments